Hmm … it looks like your browser is out of date.
Let’s update your browser so you can enjoy a faster, more secure site experience.
Don't lose benefits
You can update your information online with ePASS. ePASS is North Carolina’s secure self-service website where you can apply for various benefits, view your case details, renew your Medicaid and update your information without having to visit your local DSS. If you have an account, log in and update your information as soon as possible. Learn how to create an account here: What is ePASS?
More information can be found here: medicaid.ncdhhs.gov/renew. If you want to learn more about Medicaid recertification (renewal), check out our Recertification Fact Sheet.
We are here for you, North Carolina
We’re here to help make things a little easier. That’s why our Medicaid health plan includes so many extras for your health and everyday life.
Helping people is at the heart of all we do
Get the Medicaid plan that gives you more. All North Carolinians deserves affordable health care, including you. That includes adults, people with disabilities, pregnant women and children. UnitedHealthcare has services and extras that can make a real difference in your life.
Plus, we offer one of the largest provider networks in North Carolina. Which gives you many options to choose the doctors and specialists that fit your health care needs.
NC DHHS announced that Medicaid Expansion is planned to start October 1, 2023. The launch depends on the NC General Assembly acting by September 1. State takes action to start Medicaid Expansion Oct. 1; Launch depends on General Assembly acting by Sept. 1
We’re here to help you feel healthy and happy
At UnitedHealthcare Community Plan of North Carolina, we believe Medicaid benefits includes more than just medical services. Our Medicaid benefits include support for your whole self — body, mind and spirit. Because feeling well comes from feeling whole.
View the videos below to learn more about UnitedHealthcare Medicaid.
Video transcript
Ernestine Surgeon:
I've already had wonderful experiences when I called and needed new meter. I'm a diabetic. Soon as I called, everything I said, she was like, “Don't worry, we got a company. They take care of us very well.” Got my meter in a couple of days and they were able to get my doctor to okay the amount of strips that I needed. So it’s the little things that actually make your day better and makes your life more complete.
Video transcript
Cammeader Hammie:
I know myself, they keep me updated with extra benefits that we can do when we go to the doctor's office. They call. I have gotten some calls to check on me to see how I was doing. They gave me information where I can call them back if I need any help or problems I might have or support I might need. Just a phone call makes you say, okay they really, really care about me. They called me to check up on me and I usually don't get that from a health service person. So that is good.
Video transcript
If you've got Medicaid make sure medicaids got you too, by keeping your contact information up to date every year Medicaid has to confirm your eligibility. That means we need to be able to reach you with information or questions. You'll get a letter letting you know what we need or that your coverage has been automatically renewed.
If we don't have what we need, we'll contact you to provide any missing information reply right away. So you can keep your Medicaid coverage. If you're no longer eligible for Medicaid, we'll send you a letter about other health coverage options and financial help that can lower your cost.
Four out of five consumers can find coverage for less than $10 a month. And all plans cover things like prescription drugs doctor visits hospital stays Mental Health Services and more. Don't wait whether you still qualify for Medicaid or not. Make sure you have a plan to stay covered.
Keep your health keep your coverage.
Video transcript
What makes us different is our people. The commitment that our people have to meeting the needs of the individuals that we serve. That's what I love about United HealthCare. That's what I love about our team in North Carolina is our commitment to people, our commitment to working with stakeholders to really make the health care system better for everyone.
Every individual has different needs. Every individual has different challenges.
Was very proud and excited to be a part of United Healthcare. I've already had wonderful experiences when I called and needed a new meter. I'm a diabetic. Soon as I called everything I said she was like, “Don't worry, we got a company. They take care of us very well.” Got my meter in a couple of days and they were able to get my doctor to okay the amount of strips that I needed.
So it’s the little things that actually make your day better and makes your life more complete.
They call. I have gotten some calls to check on me to see how I was doing. They gave me information where I can call them back if I need any help or problems I might have or support I might need. Just a phone call makes you say, okay they really, really care about me. They called me to check up on me and I usually don't get that from a health service person.
So that is good.
20% of a person's health is based on health care services that they receive from their physician, from their hospital. The other 80% is based on what’s referred to as social determinants of health. Those are their non-medical or non health issues, things like transportation, having a job, access to good healthy foods. United Healthcare is committed to ensuring that we address and close those social determinants of health issues.
Some of the things that we have been doing and that we continue to do, one around food insecurity.
Well, the support from United Healthcare is really tremendous because it will be transformational from the standpoint of enabling us to bring food where it's needed most. Fresh fruits and vegetables are difficult to access for many families because of cost and even transportation. And having a mobile pantry that can bring food where it's needed most, as well as basically eliminating both the transportation issue as well as the cost issue, is really a game changer for families.
They really stand on the grounds with us being boots on the ground to help meet those growing needs in the community. And with the economy right now coming out of the pandemic, our needs have grown even more. And because of United Healthcare, we could continue to stand on the front lines against hunger and meet immediate emergency needs of our community.
You know, as we think about our mission of helping people live healthier lives and making the health care system work better for everyone, the reality is no one can do it alone. Our commitment is continued collaboration and work with our physicians, with our hospitals, with our faith based organizations, our community based organizations, many, many and all entities that impact health in any way.
It takes all of us working together to make it happen. And so I'm really excited about the progress we've made. But more to come.
UnitedHealthcare Community Plan Medicaid
Your extra benefits may include

Member information
Member handbooks
Member handbook - English
Member handbook - Español
Member services:
1-800-349-1855 / TTY 711
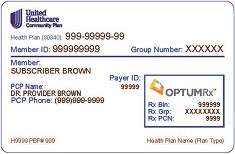
Sign in and you'll get tools that help you use your plan. You can view your Member ID card and get help with using your benefits. It just takes a few minutes to register. Then you can log in anytime.

How to enroll
1. Online - www.ncmedicaidplans.gov
2. Phone - 1-833-870-5500 (TTY 1-833-870-5588), 7 a.m. to 5 p.m., Monday through Saturday
3. Mail - Fill out the enrollment form you receive in the mail.
4. Mobile app - Download the free mobile app - NC Medicaid Managed Care
5. Need help - If you want help choosing a plan, an independent team of enrollment specialists can give you more information about the health plans available to you. Call an enrollment specialist at 1-833-870-5500 (TTY 1-833-870-5588) or visit www.ncmedicaidplans.gov.
Featured programs and benefits

Depression and anxiety
Depression is a real illness. It can be treated.
You can feel like yourself again. Depression is an illness like diabetes or heart disease. The first step is to accept that you need help. The second step is to talk to your doctor or provider.
Note: If you or someone you know is in suicidal crisis or emotional distress, get emergency help right away.
Call 911 or Call the National Suicide Prevention Lifeline for 24/7, free and confidential support. Call 1-800-273-8255 and 1-800-799-4889 (TTY)
Common signs of depression can include:
- Feeling unhappy, down or sad every day or feeling worthless, guilty, helpless or hopeless.
- Loss of interest in hobbies, activities and people you once enjoyed.
- Trouble sleeping or sleeping more than usual, or feeling tired, weak or low in energy.
- Loss of appetite or eating too much.
- Having trouble concentrating, remembering or making decisions.
- Thinking or talking about suicide.
Find out more online at liveandworkwell.com.

Virtual care – Doctor Chat
- 24/7 access to live virtual visits with a doctor
- Get the answers, treatment and follow-up care you need - at no cost to you
- To download the app, search for “UHC Doctor Chat” on the App Store® or Google Play®, or visit www.uhcdoctorchat.com
- Receive up to six virtual breastfeeding visits. For more information or to book an appointment, text UHCNC4MILK to 1-888-458-1364, visit www.simplifed.com/united-nc, or call 1-844-799-0538.
- Participate in virtual pregnancy support groups. Visit momandbaby.wellhop.com to learn more.

Well and sick care
Get the care you need to stay healthy — or to get better if you are injured or sick. Member benefits include:
- Care Coordinator. Someone to coordinate the services and care you need for your health.
- Choice of Doctor. Find a doctor you trust in our network.
- Hospitalization. You pay nothing for care in a hospital.
Read more
- Lab and X-rays. Lab tests, x-rays and diagnostic imaging are covered.
- Medicines. Fill prescriptions at local pharmacies.
- Nurse Hotline. Speak with a registered nurse 24/7.
- Pregnancy Care. Extra care and support for both you and your baby.
- Shots and Vaccines. Routine shots to help protect against illness.
- Therapy Services. Physical or other therapy to help you be your best.
- Well Visits. Annual physical exams, checkups, shots and lab tests.
- Unlimited Doctor Visits. See your doctor as often as needed.
- Urgent Care. Convenient care for a sudden illness or injury.

Mother and baby
Nothing is more important than the health and well-being of a mother and her baby. That’s why member benefits include:
- Prenatal Visits. Care for you before your baby is born.
- Get a car seat ($105 value)
- Electric breast pump ($250 value) Breastfeeding Support ($650 value). Receive up to six virtual breastfeeding visits. For more information or to book an appointment, text UHCNC4MILK to 1-888-458-1364, visit www.simplifed.com/united-nc, or call 1-844-799-0538.
- Community-Based Doula Programs ($1,200 value)
Read more
- Community baby showers with gifts, resources, and education $100 in rewards for baby products
- Healthy First Steps® Rewards. Get extra support and rewards to keep you and your baby healthy. Visit www.uhchealthyfirststeps.com for more information.
- Text4baby. Receive text messages with helpful tips and reminders.
- Wellhop. Participate in virtual pregnancy support groups. Visit momandbaby.wellhop.com to learn more.

Care for conditions
If you have asthma, diabetes or another long-term condition, you can depend on us. Our plan makes sure you get the care and services you need. Benefits include:
- Asthma and Allergies Care. Exams, testing and supplies are covered.
- Care Management. If you qualify, get personal help managing health conditions.
- Diabetic Support. Medicine, needles, wipes and other supplies for managing diabetes.
- Kidney Disease Care. Dialysis, medicine and treatments are covered.
- Behavioral Health Disorders. Counseling and other treatments are covered.
- Obesity Care. We cover screenings and counseling for obesity
- Special Needs Unit. Services for members with special health care needs.
Vision, speech and hearing care
Make sure your sight and hearing are at their best. Benefits include:
- Hearing. Tests, checkups and hearing aids, if needed, are provided.
- Vision. Covers eye exams and glasses if needed.

Transportation
Emergency: If you need emergency transportation (an ambulance), call 911.
Non-emergency: UnitedHealthcare Community Plan of North Carolina can arrange and pay for your transportation to help you get to and from your appointments for Medicaid-covered care. This service is free to you. If you need an attendant to go with you to your doctors appointment, or if your child (18 years old or younger) is a member of the plan, transportation is also covered for the attendant, parent or guardian. Non-emergency transportation includes personal vehicles, taxis, vans, mini-buses, mountain area transports and public transportation.
How to get non-emergency transportation. Call 1-800-349-1855, TTY 711 up to 2 days before your appointment to arrange transportation to and from your appointment.
Read more
Non-emergency transportation services via personal vehicles, taxis, vans, mini-buses, mountain area transports and public transportation are provided through our contracted transportation company ModivCare. You can contact ModivCare to request or cancel a trip by calling Member Services at 1-800-349-1855, TTY 711 and choosing the option for Transportation. Rides for routine appointments should be scheduled at least 2 business days in advance by calling between 7:00 a.m. and 6:00 p.m., Monday through Saturday. Rides for urgent appointments can also be made after hours by calling Member Services.
Responsibilities of the member:
- To use those transportation resources which are available and appropriate to their needs in the most efficient and effective manner.
- To utilize transportation services, such as gas vouchers, appropriately.
- To travel to the requested location and receive a Medicaid covered service.
- To make timely requests for transportation assistance.
- To be ready and at the designated place for transportation pick-up or cancel the transportation request timely.
- To follow the instructions of the driver.
- To respect and not violate the rights of other passengers and the driver, such as not creating a disturbance or engaging in threatening language or behavior.
Member no-shows:
- A no-show is when the member does not go to the medical appointment.
- The member must be ready and at the designated place for pick-up at the time required by the transportation vendor.
- The member must complete their trip and show evidence in order to be issued reimbursement for their mileage.
- The member must call the number provided for trip requests to cancel scheduled transportation at least 24 hours in advance.
- Members who miss three or more trips in a three-month period, or who risk the safety of other passengers or the driver may be suspended from transportation services for up to 30 days.
- You can get additional information on our Non-Emergency Medical Transportation policy by calling Member Services at 1-800-349-1855, TTY 711.
To view the UnitedHealthcare Community Plan of North Carolina NEMT Policy click here

Other extras for members
Sometimes you might need a little extra help using your health plan. For those times, you can rely on:
- Healthy First Steps® Rewards. Earn rewards for keeping you and your baby healthy.
- Language Help. Connect to a translator through Member Services.
- Member Advocate. Someone to get you information, services and care.
- Nurse Hotline. Speak with a registered nurse 24/7.
- Quitting Tobacco. Coaches and supplies to help you quit using tobacco.
- Social Services. We’ll help you find community services.
- Transportation. We pay for rides to and from medical visits or qualified trips to the Pharmacy.
- Weight Control. Support and treatment to reach a healthy weight.
Health education
Learn about plan types
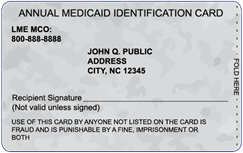
Medicaid plans
Medicaid is health insurance for people with low incomes. You might be able to get Medicaid if you're pregnant, have children or live with a disability. In some cases, other adults also may qualify. Costs to you are low and based on your ability to pay. It's important to know that Medicaid rules and coverage differ from state to state.
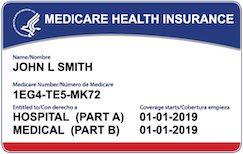
Dual Special Needs (D-SNP plans)
Medicaid is health insurance for people with low incomes. You might be able to get Medicaid if you're pregnant, have children or live with a disability. In some cases, other adults also may qualify. Costs to you are low and based on your ability to pay. It's important to know that Medicaid rules and coverage differ from state to state.
Individual and Family plans
Individual and Family Plans, also known as the Health Insurance Marketplace (R) plans, help individuals, families, and small businesses shop for and enroll in affordable healthcare coverage. Whether you qualify for these programs depends on your expected income, household members, and other information.
Don't lose benefits
You can update your information online with ePASS. ePASS is North Carolina’s secure self-service website where you can apply for various benefits, view your case details, renew your Medicaid and update your information without having to visit your local DSS. If you have an account, log in and update your information as soon as possible. Learn how to create an account here: What is ePASS?
More information can be found here: medicaid.ncdhhs.gov/renew. If you want to learn more about Medicaid recertification (renewal), check out our Recertification Fact Sheet.